Embarking on the journey of parenthood is an extraordinary chapter in the lives of individuals and couples alike. Pregnancy, a miraculous and complex biological process, marks the inception of this transformative expedition. It is a period characterized by profound physical, emotional, and psychological changes, both for the expectant mother and her partner.
Disclaimer
The information provided in this article is for general informational purposes only and is not intended as medical advice. Every pregnancy is unique, and individual circumstances may vary. It is crucial to consult with qualified healthcare professionals for personalized guidance and care tailored to specific needs.
1. Introduction
1.1 Overview of Pregnancy

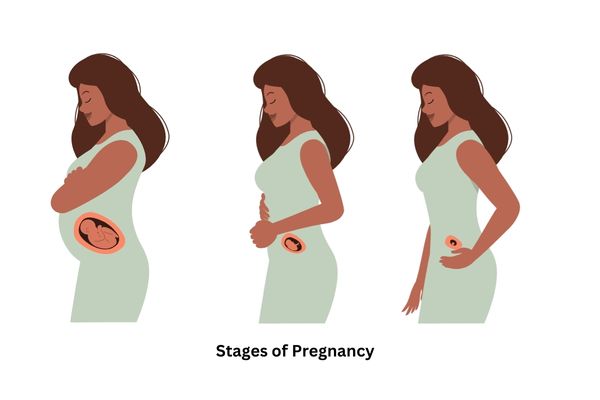
Often lasting around 40 weeks, pregnancy is a miraculous course where a single fertilized egg evolves into a fully formed infant. Divided into three distinct trimesters, each spanning approximately three months, this intricate process involves intricate interplays of hormones, cellular growth, and physiological adjustments. From the initial stages of conception to the miraculous moment of childbirth, the journey is a testament to the marvels of the human body.
Understanding the stages of pregnancy necessitates a closer look at the milestones and developments occurring within each trimester. From the delicate formation of vital organs during the first trimester to the maturation of bodily systems in the second and the final preparations for birth in the third, comprehending this chronological progression is vital for expectant parents to navigate this transformative period with confidence and knowledge.
1.2 Importance of Understanding Pregnancy Stages
The significance of comprehending the stages of pregnancy cannot be overstated. Knowledge empowers, and in the case of pregnancy, it enables prospective parents to make informed decisions about their health and well-being. Understanding the nuances of each stage allows for proactive health management, early identification of potential complications, and establishing a supportive environment for the growing life within.
Beyond the realm of physical health, a nuanced understanding of pregnancy stages contributes significantly to expectant parents’ emotional and psychological well-being. It fosters a connection with the unborn child, promotes shared responsibility between partners, and helps build a foundation for a healthier transition into parenthood.
In this comprehensive guide, we delve into the intricate tapestry of pregnancy, unraveling the mysteries of each trimester and shedding light on the diverse facets of this remarkable journey. From preconception considerations to postpartum adjustments, our exploration aims to equip readers with the knowledge and insight needed to navigate the stages of pregnancy with confidence and grace.
Also check: When is the worst time to drink during pregnancy?
2. Preconception Phase
The preconception phase plays a crucial role in the journey to parenthood, setting the stage for a healthy and successful pregnancy. During this period, couples can take proactive steps to optimize their health, addressing physical and lifestyle factors that can influence fertility and the well-being of the future baby.
2.1 Importance of Preconception Care
Preconception care is not merely a formality but a strategic approach to ensure the best possible conditions for conception and healthy pregnancy. This phase involves making lifestyle adjustments and seeking medical guidance before attempting to conceive. The significance of preconception care lies in its ability to:
- Enhance Fertility: By addressing factors such as nutrition, weight, and overall health, preconception care can boost fertility, increasing the chances of successful conception.
- Minimize Pregnancy Risks: Identifying and managing pre-existing health conditions, such as diabetes or hypertension, can significantly reduce the risks associated with pregnancy.
- Promote a Healthy Start: The health of both partners before conception can influence the baby’s development from the earliest stages, potentially preventing certain congenital conditions.
- Optimize Reproductive Health: Preconception care allows for the detection and treatment of reproductive health issues, ensuring that both partners are in their best possible reproductive condition.
2.2 Lifestyle and Dietary Considerations
A key aspect of preconception care involves adopting a healthy lifestyle and making dietary choices that support reproductive health. Couples should consider:
- Balanced Nutrition: A diet rich in vitamins, minerals, and essential nutrients is vital for reproductive health. Folic acid, for example, is crucial in preventing neural tube defects in the developing fetus.
- Maintaining a Healthy Weight: Both underweight and overweight conditions can affect fertility. Achieving and maintaining a healthy weight contributes to overall well-being and fertility.
- Limiting Exposure to Harmful Substances: Smoking, excessive alcohol consumption, and drug use can negatively impact fertility and increase the risk of birth defects. Preconception is the ideal time to quit such habits.
- Regular Exercise: Engaging in moderate physical activity promotes overall health and helps manage stress and maintain a healthy weight, contributing to optimal fertility.
2.3 Preconception Health Checkups
Before conception, both partners should undergo comprehensive health checkups. These checkups may include the following:
- Screening for Infectious Diseases: Identifying and treating infections, such as sexually transmitted diseases, can prevent complications during pregnancy.
- Genetic Counseling: Understanding potential genetic risks allows couples to make informed decisions and, if necessary, explore options such as genetic testing.
- Reviewing Medications: Some medications may pose risks during pregnancy. A healthcare provider can assess current medications and recommend adjustments as needed.
- Assessment of Reproductive Health: Both partners may undergo tests to assess fertility and reproductive health, identifying any issues that could affect conception.
In essence, the preconception phase is a proactive and empowering stage, allowing couples to take control of their health and make informed decisions that positively impact their fertility and the well-being of their future child. Through preconception care, individuals set the foundation for a healthy and fulfilling pregnancy journey.
3. First Trimester: Weeks 1-12
3.1 Early Signs of Pregnancy
Discovering you’re pregnant often begins with subtle but telling signs. During the early weeks of pregnancy, your body undergoes significant changes. Some common early signs include:
- Missed Period: One of the most obvious signs is a missed menstrual period. If your periods are regular, a missed period can be a strong indicator of pregnancy.
- Morning Sickness: Nausea and vomiting, commonly referred to as morning sickness, can strike at any time of the day. Hormonal changes often trigger this.
- Fatigue: Feeling more tired than usual is another early sign. The body is working hard to support the growing embryo, and it can lead to increased fatigue.
- Breast Changes: Tender and swollen breasts are typical as hormone levels rise. You might notice changes in nipple color and sensitivity.
- Frequent Urination: Hormonal shifts and the expanding uterus can lead to increased frequency of urination. It is a common symptom that may persist throughout pregnancy.
- Mood Swings: Hormonal fluctuations can impact your mood, causing mood swings ranging from joy to irritability.
3.2 Development of the Embryo
During the first trimester, the embryo undergoes rapid development. Key milestones include:
- Weeks 1-4: Fertilization occurs, and the zygote begins to divide and form a blastocyst. This tiny ball of cells implants itself in the uterine lining.
- Weeks 5-8: Major organs and body structures start to form. The heart begins to beat, and facial features, limbs, and vital organs develop.
- Weeks 9-12: The embryo is now called a fetus. By the end of the first trimester, the fetus has developed all significant organs and systems, including fingers, toes, and external genitalia.
3.3 Changes in the Mother’s Body
As the embryo grows, the mother’s body undergoes significant changes to support the pregnancy:
- Uterine Expansion: The uterus expands to accommodate the growing embryo, which may cause mild cramping.
- Hormonal Changes: Elevated levels of hormones, including human chorionic gonadotropin (hCG) and progesterone, contribute to various symptoms like nausea, breast changes, and mood swings.
- Blood Volume Increase: Blood volume increases, leading to blood pressure changes and increased heart workload.
- Weight Gain: Some women may experience slight weight gain due to hormonal changes and increased blood volume.
3.4 First Trimester Health Tips
Taking care of yourself during the first trimester is crucial for a healthy pregnancy:
- Prenatal Care: Schedule your first prenatal appointment to monitor the health of both you and the baby.
- Nutrition: Focus on a well-balanced diet rich in essential nutrients, including folic acid, iron, and calcium. Consult with your healthcare provider about prenatal supplements.
- Hydration: Drink plenty of water to stay hydrated, especially if you’re experiencing morning sickness.
- Rest: Your body is working hard to support the pregnancy. Ensure you get adequate rest and sleep.
- Avoid Harmful Substances: Steer clear of alcohol, tobacco, and recreational drugs. Consult your healthcare provider about medications.
- Emotional Well-being: Pregnancy can be emotionally challenging. Seek support from loved ones and consider joining prenatal classes or support groups.
Remember, each pregnancy is unique, and you must communicate openly with your healthcare provider about any concerns or questions you may have during this transformative time.
4. Second Trimester: Weeks 13-27
The second trimester of pregnancy is often hailed as the “golden period” for many expectant mothers. During these weeks, from the 13th to the 27th week, significant developments unfold for both the growing fetus and the mother’s evolving body. A sense of relief marks this phase for many women as the initial challenges of the first trimester subside and the joys of impending motherhood become more tangible.
4.1 Growth and Development of the Fetus
In this crucial phase, the fetus undergoes remarkable transformations. Organs and structures continue to form, and by the midpoint of the second trimester, the fetus is unmistakably human in appearance. Tiny fingers and toes develop, and the baby begins to exhibit reflexes. The skeleton, initially soft cartilage, begins to harden into bone. By week 20, the mother may even start feeling those gentle flutters of movement, a delightful sensation marking the early stages of fetal activity.
The latter part of the second trimester witnesses rapid brain development, setting the stage for sensory experiences. The fetus can hear sounds from the external environment, making it an ideal time for parents to talk or sing to their unborn child. The second trimester serves as a critical period for fetal growth and lays the foundation for the upcoming stages of pregnancy.
4.2 Maternal Physical and Emotional Changes
Expectant mothers experience a shift in their physical and emotional well-being during the second trimester. For many, the initial nausea and fatigue begin to wane, replaced by a surge of energy and vitality. The infamous “baby bump” becomes more pronounced, eliciting a sense of excitement and connection to the growing life within.
Emotionally, many women find a newfound sense of well-being during this trimester. Hormonal fluctuations stabilize, reducing mood swings and anxiety. The second trimester often brings a sense of euphoria and connection as the reality of impending motherhood sets in. However, it’s essential to acknowledge that emotional experiences can vary, and each woman’s journey is unique.
4.3 Common Second Trimester Discomforts
While the second trimester is generally more comfortable than the first, certain discomforts may persist. Backaches are expected as the belly expands and the center of gravity shifts. Leg cramps and swelling can occur, emphasizing the importance of proper hydration and regular movement. Some women may experience skin changes, such as darkening of the skin or the appearance of a linea nigra—a dark line running down the abdomen.
It’s common for nasal congestion and bleeding gums to appear due to increased blood flow. Additionally, the pressure on the bladder intensifies, leading to frequent bathroom trips. While these discomforts are part of the journey, maintaining open communication with healthcare providers ensures proper management and support.
4.4 Nutrition and Exercise Recommendations
Nutrition plays a pivotal role in supporting the well-being of both mother and baby during the second trimester. A well-balanced diet rich in essential nutrients such as folic acid, iron, calcium, and omega-3 fatty acids is crucial for fetal development. Prenatal vitamins may be recommended to fill potential nutritional gaps.
Moderate and regular exercise is encouraged, promoting overall health and aiding in the management of common discomforts. Walking, swimming, and prenatal yoga can enhance flexibility and stamina. Consultation with a healthcare provider is essential to tailor exercise routines to individual needs and circumstances.
In conclusion, the second trimester is a transformative period characterized by fetal growth, maternal well-being, and a deepening connection to the miracle of life. Understanding these changes empowers expectant parents to navigate this journey with knowledge and anticipation.
5. Third Trimester: Weeks 28-40

The third trimester marks the final stretch of the incredible pregnancy journey, bringing both anticipation and a whirlwind of changes for the growing baby and the expectant mother.
5.1 Fetal Development in the Final Weeks
As the delivery countdown begins, fetal development peaks during the third trimester. The baby now significantly more prominent undergoes crucial developments to prepare for life outside the womb. Organs and systems continue to mature, with particular emphasis on lung development. The baby’s bones, initially soft, begin to harden, and fat accumulates under the skin, providing insulation and energy reserves. By the end of this trimester, the baby is positioned for birth, with the head typically pointing downward.
Understanding these intricate changes aids in appreciating the delicate balance of growth within the womb. Expectant parents often marvel at the ultrasound images that reveal the baby’s features, fostering a more profound connection as they eagerly await the upcoming arrival.
5.2 Maternal Changes and Challenges
The third trimester heralds joyous anticipation and a host of physical changes for the mother. The growing baby places increased pressure on internal organs, potentially leading to discomfort, heartburn, and difficulty sleeping. Swelling in the extremities, known as edema, becomes more pronounced due to fluid retention.
Moreover, as the body prepares for labor, there may be an increase in Braxton Hicks contractions, a phenomenon where the uterus tightens and relaxes, often mistaken for actual labor. Backaches and pelvic pain may also intensify as the body readies itself for childbirth. Amidst these challenges, maintaining open communication with healthcare providers ensures proper monitoring and support for a smoother transition.
5.3 Preparing for Labor and Delivery
With the due date on the horizon, preparation for labor and delivery becomes a focal point. Expectant parents discuss the birthing process, exploring various birthing options and pain management techniques. This period often involves creating a birth plan, a document that outlines preferences for labor, delivery, and postpartum care.
Understanding the signs of labor, such as contractions and the rupture of membranes, empowers parents to make informed decisions about when to head to the hospital or birthing center. Familiarizing oneself with the stages of labor contributes to a sense of readiness and confidence as the momentous day approaches.
5.4 Antenatal Classes and Birth Plans
Antenatal classes are pivotal in equipping expectant parents with the knowledge and skills necessary for labor, delivery, and early parenthood. These classes cover various topics, including breathing techniques, pain management strategies, and postpartum care. Attending these classes fosters a supportive community among soon-to-be parents, providing a platform to share experiences and concerns.
Simultaneously, crafting a birth plan allows expectant parents to communicate their preferences to healthcare providers, ensuring a personalized and respectful birthing experience. From choices about pain relief to preferences for the immediate postpartum period, a well-thought-out birth plan serves as a valuable guide amid the unpredictability of childbirth.
In essence, the third trimester embodies a period of intense preparation and transformation, both for the baby and the expectant mother. By navigating these final weeks with knowledge and support, parents set the stage for a positive and empowered birthing experience.
6. Common Pregnancy Complications

6.1 Gestational Diabetes: Gestational diabetes is a type of diabetes that occurs during pregnancy, typically around the 24th week. It develops when the body cannot produce enough insulin to meet the increased demands, leading to elevated blood sugar levels. This condition poses risks for both the mother and the baby. Complications may include:
- Macrosomia (a larger-than-average baby).
- Preterm birth.
- An increased likelihood of cesarean delivery.
Regular monitoring of blood sugar levels, dietary modifications, and sometimes medication are critical components of managing gestational diabetes. Early detection and proper management can contribute to a healthy pregnancy outcome.
6.2 Pre-eclampsia: Pre-eclampsia is a severe condition characterized by high blood pressure and damage to organs, often the liver and kidneys, after 20 weeks of pregnancy. It can lead to complications such as premature birth and low birth weight, and in severe cases, it may threaten the life of both the mother and the baby. Regular prenatal checkups, monitoring blood pressure, and urine tests are essential for early detection. Treatment may involve medication, bed rest, and close medical supervision. In severe cases, early delivery might be necessary to protect the health of both mother and baby.
6.3 Placenta-related Issues: Issues with the placenta, such as placenta previa and placental abruption, can pose significant risks during pregnancy. Placenta previa occurs when the placenta partially or completely covers the cervix, potentially causing bleeding and complications during delivery. Placental abruption involves the detachment of the placenta from the uterine wall, leading to bleeding and potential oxygen deprivation for the baby. Both conditions require close monitoring and may necessitate medical intervention, ranging from bed rest to emergency delivery depending on the severity.
6.4 Recognizing and Managing Complications: Recognizing the signs of pregnancy complications is crucial for prompt intervention. Symptoms like persistent abdominal pain, severe headaches, visual disturbances, or decreased fetal movement should not be ignored. Regular prenatal checkups, ultrasound examinations, and blood tests help healthcare providers monitor the health of both the mother and the baby. In the event of complications, a collaborative approach between the patient, healthcare providers, and specialists may be necessary to tailor a management plan that ensures the best possible outcome for both.
7. Nutritional Requirements During Pregnancy
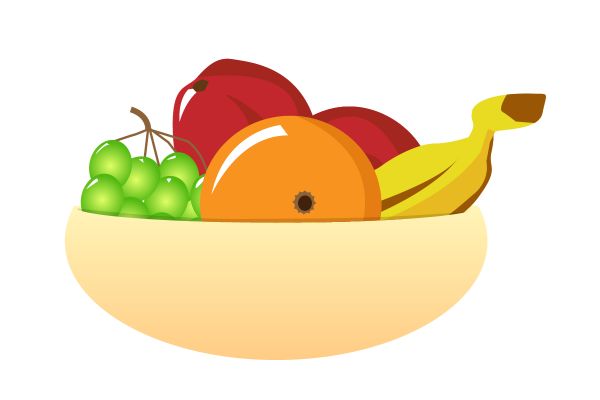
7.1 Importance of a Balanced Diet: Maintaining a balanced diet during pregnancy is paramount for the health and well-being of the mother and the developing baby. A diverse and nutritious diet provides essential vitamins, minerals, and nutrients for fetal growth and development. Proper nutrition also supports the mother’s overall health, reducing the risk of complications such as gestational diabetes and pre-eclampsia. A diet rich in fruits, vegetables, lean proteins, whole grains, and dairy ensures that pregnancy’s nutritional and caloric needs are met.
7.2 Key Nutrients for Fetal Development: Several critical nutrients play a vital role in fetal development. Folic acid, iron, calcium, omega-3 fatty acids, and vitamin D are crucial elements that contribute to the development of the baby’s brain, bones, and overall health. Prenatal supplements, as recommended by healthcare providers, are often prescribed to bridge potential nutritional gaps. Adequate hydration is essential for maintaining amniotic fluid levels and supporting the increased blood volume during pregnancy.
7.3 Foods to Avoid During Pregnancy: While a balanced diet is essential, there are certain foods that pregnant women should avoid to minimize the risk of complications. Raw or undercooked seafood, unpasteurized dairy products, and high-mercury fish should be limited or excluded. Caffeine intake should be moderated, and alcohol consumption is strongly discouraged as it can lead to birth defects. Additionally, certain types of soft cheeses and deli meats may risk bacterial contamination. Consulting with healthcare providers for personalized dietary advice is crucial to ensure a safe and healthy pregnancy.
8. Prenatal Care and Medical Checkups

8.1 The Role of Prenatal Visits: Prenatal visits play a pivotal role in ensuring the health and well-being of the mother and the developing baby throughout pregnancy. These regular checkups, typically scheduled monthly during the first two trimesters and more frequently in the third, allow healthcare providers to monitor the progress of the pregnancy. During these visits, healthcare professionals assess vital signs, track weight gain, and perform routine tests to identify potential complications early on. The collaborative relationship between the expectant mother and her healthcare team ensures that any emerging issues can be addressed promptly, contributing to a safer and healthier pregnancy.
8.2 Ultrasound Scans and Tests: Ultrasound scans and various diagnostic tests are integral to prenatal care, offering invaluable insights into the developing fetus. Ultrasounds visually confirm the baby’s growth, development, and overall health. Diagnostic tests such as amniocentesis or blood screenings may also be recommended based on specific risk factors. These tests help identify potential genetic abnormalities or other health concerns, allowing for informed decision-making and tailored care plans. By incorporating advanced medical technologies, prenatal care strives to provide a comprehensive understanding of the baby’s health while reassuring expecting parents.
8.3 Monitoring the Mother’s and Baby’s Health: Continuous monitoring of both the mother’s and baby’s health is a cornerstone of prenatal care. Regular assessments of blood pressure, heart rate, and other vital signs help detect and manage conditions such as gestational diabetes or pre-eclampsia. Monitoring fetal movements and heart rate helps ensure the baby’s well-being. Through a combination of physical examinations, lab tests, and cutting-edge diagnostic tools, healthcare providers work to create a supportive environment, addressing any emerging concerns promptly. This comprehensive approach optimizes maternal health and fetal development, contributing to a successful and safe pregnancy.
9. Emotional and Psychological Well-being

9.1 Coping with Hormonal Changes: Pregnancy brings about a cascade of hormonal changes that can significantly impact a pregnant mother’s emotional well-being. Understanding and coping with these changes is crucial for a positive pregnancy experience. Hormonal fluctuations can contribute to mood swings, heightened emotions, and even feelings of anxiety or depression. Open communication with healthcare providers, participating in prenatal classes, and seeking emotional support from loved ones can help mothers navigate these changes with resilience and empowerment.
9.2 Building a Support System: Building a robust support system is paramount for expectant mothers as they navigate the emotional and physical demands of pregnancy. This support system may include a partner, family, friends, and healthcare professionals. Establishing open lines of communication, expressing needs and concerns, and sharing the journey with those who care can alleviate stress and contribute to a positive emotional state. Support groups and counseling services are also valuable resources, providing a platform for connecting with others experiencing similar emo.
Emotional state. Support groups and counseling services are also valuable resources, providing a platform for connecting with others experiencing similar emotions and challenges.
9.3 Addressing Anxiety and Stress: Anxiety and stress are familiar companions during pregnancy, but addressing these challenges is crucial for both maternal and fetal well-being. Techniques like mindfulness, relaxation exercises, and prenatal yoga can help manage stress levels. Effective communication with healthcare providers about emotional struggles ensures timely intervention and support. In some cases, counseling or therapy may be recommended to provide a structured space for addressing anxiety or stressors. Expectant mothers can cultivate a positive mindset and foster a healthier environment for themselves and their developing babies by prioritizing emotional well-being.
10. Preparing for Labor and Delivery

10.1 Signs of Approaching Labor: Recognizing the signs of approaching Labor is essential for expectant parents. These signs may include changes in the baby’s position, the onset of regular contractions, or the amniotic sac rupture. Understanding these indicators empowers parents to decide when to head to the hospital or birthing center. Prenatal education classes often cover these signs in detail, providing expectant parents with the knowledge and confidence needed as they anticipate the exciting arrival of their newborn.
10.2 Types of Delivery Understanding the various types of delivery is a crucial aspect of preparing for Labor. Vaginal births, cesarean sections, and assisted deliveries are among the options, each with its considerations and potential scenarios. Prenatal education and discussions with healthcare providers help expectant parents make informed decisions about their preferred delivery method. This knowledge ensures that the birthing experience aligns with the mother’s preferences and medical considerations, fostering a sense of control and preparedness.
10.3 Packing a Hospital Bag: Packing a hospital bag well before the due date is a practical and reassuring step for expectant parents. This bag typically includes essentials for the mother and baby during their hospital stay. Items such as comfortable clothing, toiletries, important documents, and baby essentials are commonly recommended. Creating a checklist and having the bag ready ensures a smoother experience when heading to the hospital, allowing parents to focus on the excitement and joy of welcoming their new addition to the family.
11. Postpartum Period

Welcoming a new life into the world marks the beginning of postpartum, a crucial phase where mothers undergo physical and emotional adjustments. Here’s a closer look at critical aspects:
11.1 Physical Recovery After Birth: The postpartum body experiences remarkable changes as it heals from childbirth. Understanding and managing these physical transitions are vital from uterine contractions to post-delivery bleeding. We explore the typical recovery timeline and offer insights into navigating the post-birth physical journey.
11.2 Emotional Well-being: Emotional well-being is at the forefront during the postpartum period. Hormonal shifts, sleep deprivation, and the demands of caring for a newborn can impact a mother’s mental health. We delve into common emotional challenges, provide coping strategies, and emphasize the importance of seeking support. Nurturing the mother’s mental health is integral to fostering a positive postpartum experience.
11.3 Postpartum Care and Support: Comprehensive postpartum care extends beyond the hospital stay. From nutrition and self-care practices to managing postpartum complications, we guide mothers through the essentials of self-nurturing. Additionally, we shed light on the crucial role of support networks, including partners, family, and healthcare professionals, in ensuring a smooth transition into motherhood.
The postpartum period is a transformative journey, and understanding its intricacies empowers mothers to embrace the challenges and joys of this unique phase in their lives.
Conclusion: Celebrating the Journey to Parenthood
In concluding our exploration of the stages of pregnancy, it’s essential to recognize the incredible journey embarked upon by expectant parents. From the delicate preconception phase to the momentous birth and beyond, each stage brings challenges and joys.
Understanding the physical and emotional transformations, navigating potential complications, and embracing the significance of prenatal care contribute to a healthier, more informed pregnancy experience. The journey doesn’t conclude with delivery; it extends into the postpartum period, where recovery and the joys of parenting begin.
As we celebrate the resilience of both mothers and fathers, it’s crucial to acknowledge the support systems that play a pivotal role. Whether it’s healthcare providers, family, or friends, the collective effort enhances the well-being of the mother and the newborn.
Ultimately, the stages of pregnancy mark the initiation of a profound, lifelong connection between parents and their child. This guide aims to empower, inform, and instill confidence in individuals navigating this transformative chapter, fostering a positive and well-prepared transition into parenthood.
Disclaimer
The information provided in this article is for general informational purposes only and is not intended as medical advice. Every pregnancy is unique, and individual circumstances may vary. It is crucial to consult with qualified healthcare professionals for personalized guidance and care tailored to specific needs.
While efforts have been made to ensure the accuracy and relevance of the content, developments in medical research and practices may lead to updates or changes. The author and publisher do not assume any responsibility for errors, omissions, or the outcome of decisions made based on the information presented in this guide.